A curious case of occlusion
by Lucy Stock

Lucy Stock presents a case that demonstrates how dentistry to address occlusion ameliorated facial dystonia spasming.
This case highlights how dentistry can influence whole body health. We are now in the exciting era of complete dentistry – the combination of dentistry, TMJ health and occlusion, nutrition, airway, sleep and overall health.
My team was captivated by this case, such that every time the patient attended, we were all eager to see what impact the dentistry had had on her condition, which was clear from the moment she set foot in reception.
Patient presentation

Denise, a 67-year-old lady, was referred to me for an implant consultation regarding her unrestorable carious root filled LL5. It was immediately apparent that she was suffering from a dystonia condition as her face was in constant motion with episodic blepharospasm (eye shutting), lip pursing, ‘Popeye’ mouth spasming to the right, tongue flicking and mandibular thrusting. It appeared exhausting with detrimental social implications.
Eleven years ago, Denise was extremely energetic and working full time in her husband’s business often coming home and continuing her paperwork late into the evening (a behaviour that she feels contributed to the onset of the condition, as her brain was continually ‘on’).
It began with one eye involuntarily closing and then the other joined in. The spasms then travelled down her face, neck and chest, and her speech became hoarse and laborious.
During the initial consultation, Denise said: ‘My eyes are shut more often than they are open, leaving me functionally blind. When I walk, I only manage to open them after every fourth step.’
It’s unsurprising that the jerking movements caused many cooking accidents, frequent bumps and trips. They made eating gruelling, meant that reading and watching TV were impossible and triggered pains that radiated from head to torso.
Diagnosis
Dystonia is an involuntary, abnormal movement and posture disorder characterised by repetitive and sustained muscle contractions. As well as motor symptoms, dystonia patients often experience isolation, depression, sleep problems, fatigue, loss of weight and pain.
A neurologist diagnosed Meige syndrome, which is the combination of blepharospasm and oromandibular dystonia. The illness is named after French neurologist Henri Meige, who published a paper on this rare (one in 100,000) dystonia syndrome in 1910.
Meige syndrome usually appears between the third and seventh decades and is more common in women by a two to one ratio (thought to be related to hormones). It’s characterised by difficulty opening the mouth, bruxism, clenching, jaw spasming, TMJ dislocation, lip tightening, increased blinking rate, squinting and photophobia.
These patients experience a higher rate of oral soft tissue trauma, tooth fracture and denture instability. The symptoms are exacerbated by stress and worse in the mornings.
The research suggests that the aetiology is a defect in the brain cells starting at the basal ganglia due to an imbalance in the neurotransmitters dopamine, acetylcholine, and gamma-aminobutyric acid.
Predental treatment
Denise had no prior medical conditions, no history of trauma and wasn’t on any medications before the onset of the dystonia. The treatment for the past 11 years had been quarterly injections of botulinum toxin to her eyes, face, neck, and base of the tongue by the neurologist.
The botulinum injections relaxed the eyes somewhat, steadied the platysma contractions and relaxed the laryngeal muscles which improved speech comprehensibility to some extent.
She also attended an osteopath who additionally performed physiotherapy and acupuncture treatments.
She took 500mcg clonazepam nightly and tried trihexyphenidyl (an anticholinergic drug used to treat tremors, spasms, and stiffness). However, the trihexyphenidyl gave severe short-term memory loss so it was stopped. She wears special glasses that stop the esotropia (inward-turning eye).
Dental exam
Normal findings
Silent TMJs when listened to by stethoscope. Opening distance 47mm. No pain on loading.
Range of motion left 13mm and right 12mm. Right lateral excursion UR2, left lateral excursion UL3. Overjet and overbite 2mm.
TMJ Piper classification one, so MRI is not indicated. The brain scans revealed nothing of note.

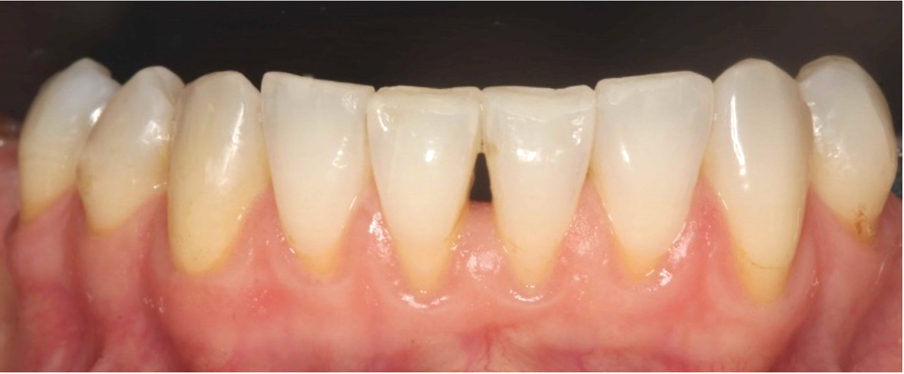

Findings of note
Mandible sitting right 2mm in maximum intercuspal position (MIP). Horizontal slide into MIP from fully seated condylar position. BEWE erosion grade 2.
Teeth not holding shim UR6 to UL2. UL7 mesiopalatal cusp was a non-working side interference. Fractured LL7 distolingual cusp. Missing LR6 and UL6.
Moderately restored dentition with poor occlusal anatomy. Suppurating periodontal abscesses UL5, UL6 and UR6.
Dental treatment
The first appointment involved full mouth professional mechanical plaque removal with ultrasonic scaler and demonstration of improved interdental cleaning techniques, which resulted in the resolution of the periodontal abscesses.
The LL5 root was extracted. The socket subsequently suppurated and was then debrided, which stimulated full healing.
All existing restorations were replaced with direct composite restorations. Under-contoured restorations were restored to more anatomically correct conformations, establishing even occlusal contacts on all teeth, incisal and canine guidance, and elimination of the interferences.
Placement of LL5 implant – still to be restored.
Supplementary treatment
After the restorative treatment, I directed her to Dr Joaquin Farias, head of the Neuroplastic Training Institute, Toronto. He treats dystonia with movement therapy and she commenced an online programme of micro facial movements for brain training with specific breathing exercises.
Also on my recommendation, she started probiotics and has continued them to date. She started taking omega-3 fish oils, has now cut out processed foods, sugar and gluten and wears a glucose monitor to regulate her blood glucose levels.
Treatment outcome
The dental treatment took four months. One month after the first restorative appointment, the facial spasms started to reduce, when the incisal edges of the LR3 to LL3 and palatal incisal surfaces of the UR3 to UL3 were bonded to restore incisal guidance.
The right-side ‘Popeye’ mouth grimacing was the first spasm to significantly reduce and this continued to improve over the following months. The eye closure diminished in frequency and intensity, although it’s still there.
The mandibular thrusting and lip pursing calmed considerably. Her speech became clearer and she was able to converse for longer without tiring. Her sleep improved. However, under stressful conditions – such as when she’s around a lot of people, when it’s windy or in bright lights – the twitching will intensify.
Pretreatment, Denise experienced daily pain in the masseter, temporalis, cervical, occipital, platysma, hyoid, SCM and ocular muscles that ranged from a four to an eight on the pain scale. Post-treatment, the muscle discomfort has reduced to once a week and ranges from a one to a five on the pain scale. The platysma pain has totally resolved. The frequency of headaches has reduced from daily to once a week. Her paracetamol intake has reduced from almost daily to once a week. She has reduced the clonazepam to once a week and before stressful outings.
Her long-term osteopath remarked that after the dental treatment, her face, neck and chest muscles felt noticeably more relaxed. Her neurologist keenly observed the quieting of the facial muscles.
Denise stated that 10 months after treatment started: ‘There has been a 60% improvement.’ She now goes for walks on her own, goes shopping by herself again and has recently booked a holiday herself and is actually looking forward to going this time.


Discussion
In 1937, Ronald P Mackay said: ‘As far as the fields of dentistry and neurology are concerned, they should be especially close […] I am convinced that every neurologist should know more dentistry, and that the average dentist would profit in many ways if he had more information about neurology.’
Before the dental treatment, Denise described her occlusion as: ‘I didn’t have anything to purchase on.’After the occlusion was re-established she said: ‘The dental treatment has made a major difference. It’s as if I have something to grip onto and it’s unlocked something in me.’
As the facial contractions reduced, Denise felt as if ‘the stability of my jaw has given me brain space to try other therapies’.
The improvement after the dental and supplementary treatment is likely multifactorial. There are close functional and anatomical relationships between cranial nerves V and VII in both their sensory and motor divisions (Sanders, 2010).
The restoration of the occlusion, resolution of the periodontal infection, osteopathy, additional dietary measures, and improved sleeping would diminish the immune system’s inflammatory reaction. This leads to a downregulation of the trigeminal and facial nerve as well as the sympathetic nervous system overall (Colucci et al, 2023) thus reducing the muscle activity similar to the mechanisms involved in complex regional pain syndrome and bruxism (Shim et al, 2019).
I recommended probiotics because gut microbiome dysbiosis has been linked to neurodegenerative disorders via the gut-brain axis and probiotics have been suggested to improve the microbiome and positively affect the brain (Timmers et al, 2023).
Aggravating factors
The relationship between dystonia and amalgam is unclear in the literature, with some studies finding that there is no correlation between muscle disorders such as essential tremors (Tseng, 2020). However, mercury has no biological function, and it has been related to the development of neuropathological conditions (Farina et al, 2013).
There may also be an element of placebo resulting from ‘the clinician’s attention’ and positive suggestions which can play a role in all patient health improvements.
Generally, the research linking oral conditions and oral mandibular dystonia is uncertain. One study concluded that, because patients with oromandibular dystonia (OMD) commonly experience TMD symptoms, they can receive a misdiagnosis of TMD while the oromandibular dystonia is overlooked (Handa et al, 2022).
The suggestion is that there’s overtreatment of unnecessary dentistry in OMD. The same study (Handa et al, 2022) found that ‘a dental procedure was a triggering or aggravating factor in 36.4% of patients’.
It would be helpful to agree on a definition of TMD and occlusion between dentists and neurologists for clinical paper comparison.
Summary
In conclusion, it may be that the two conditions are not as mutually exclusive as conventionally thought, rather, due to the complex interactions within the body there is indeed more of an overlap.
The exciting concept of complete dentistry opens the door to new treatment therapies for oromandibular dystonia and would benefit from further research.
For the references that accompany this article, email siobhan.hiscott@fmc.co.uk.
About the author
Lucy Stock, BDS Dip ImpDent RCS (Eng)
Lucy qualified from Glasgow in 1997, gained the implant diploma from RCS in 2013, and has been placing implants for 25 years. Owner of a private referral-based multidisciplinary practice in Belfast and head of Gentle Dental Training, she passes on her enthusiasm for dentistry by teaching and mentoring colleagues. Her interests are in implants, soft and hard tissue grafting, occlusion, TMD, and periodontics.
Read more Irish Dentistry clinical articles:

