Andoni Jones shares his views on techniques available to combat bone loss post extraction.
Andoni Jones shares his views on techniques available to combat bone loss post extraction.
It has been shown that 11-22% of vertical bone loss and approximately 32% of horizontal bone loss occurs in the first six months post extraction (Tan et al, 2012).
Immediate implant protocols have been developed to help minimise this bone loss as much as possible. However, implant placement itself will not stop resorption from happening. As such, clinicians have different tools available to them to improve bone volume postoperatively, including various placement techniques and biomaterials.
In Andoni Jones’ words
Every clinician has their own ideas and concepts regarding immediate implants. When a tooth is extracted, the bone and gum in the area will always shrink. Sometimes the resorption is very mild, sometimes it’s more severe – it all depends on the case.
Immediate implants do not prevent this bone loss. It’s important that this is acknowledged when immediate implant protocols are utilised and the appropriate steps are incorporated into treatment.
Very rarely will a clinician just remove a tooth, place an implant and not perform any hard or soft tissue grafting. Personally, I do not recommend this.
In my opinion, the only technique that really prevents bone loss is partial extraction therapy (PET). A portion of the root is kept in the socket, attached to the bone and therefore preventing bone loss. The implant is placed beside this root fragment.
The need for grafting materials is eliminated in this concept, but it can only be used in very few indications. For instance, it is not indicated in compromised sockets, but rather in sites with an intact buccal plate, healthy and non-fractured roots and a site free from periodontal disease or infection.
Many immediate implant candidates will not meet this criteria.
It is also important to realise that PET is a technically demanding procedure. The natural tooth has to be very precisely split into a buccal and palatal half. The palatal half has to be very carefully extracted without mobilising or damaging the buccal portion, which is shaped and reduced to create space to place the implant in the same socket. It adds another level of difficulty to immediate implants.
Other situations
Where PET is not appropriate for a case, I perform grafting procedures while utilising the right biomaterials.
There are several other potential techniques available that might be more suitable in the majority of cases. The first and longest involves extracting the tooth, placing the implant without raising a flap and performing alveolar ridge preservation or socket grafting.
This can be effective with or without the use of a soft tissue graft and it also works very well. Additionally the grafting material is added only to compensate for the tissue loss that will occur after extraction.
Another option is to extract the tooth, open a flap and graft inside the socket. Then also graft over the socket and cover this with a membrane, suturing the flap over later. For the best results, the biomaterial should remodel into natural bone in a slow and gradual process.
This minimises bone volume loss and better supports the soft tissue. It is important to understand what biomaterials can give us the best result for minimising any bone and tissue resorption.
Key to success
Selecting high-quality biomaterials is key for the success in any of these situations. It is also important to have access to a range of solutions to gain confidence in the clinical outcomes afforded in various types of immediate implant cases.
I have been using Straumann Group biomaterials for 10 years now. A wide range of clinically proven materials are available. The Straumann portfolio offers me solutions for most of my day-to-day clinical cases.
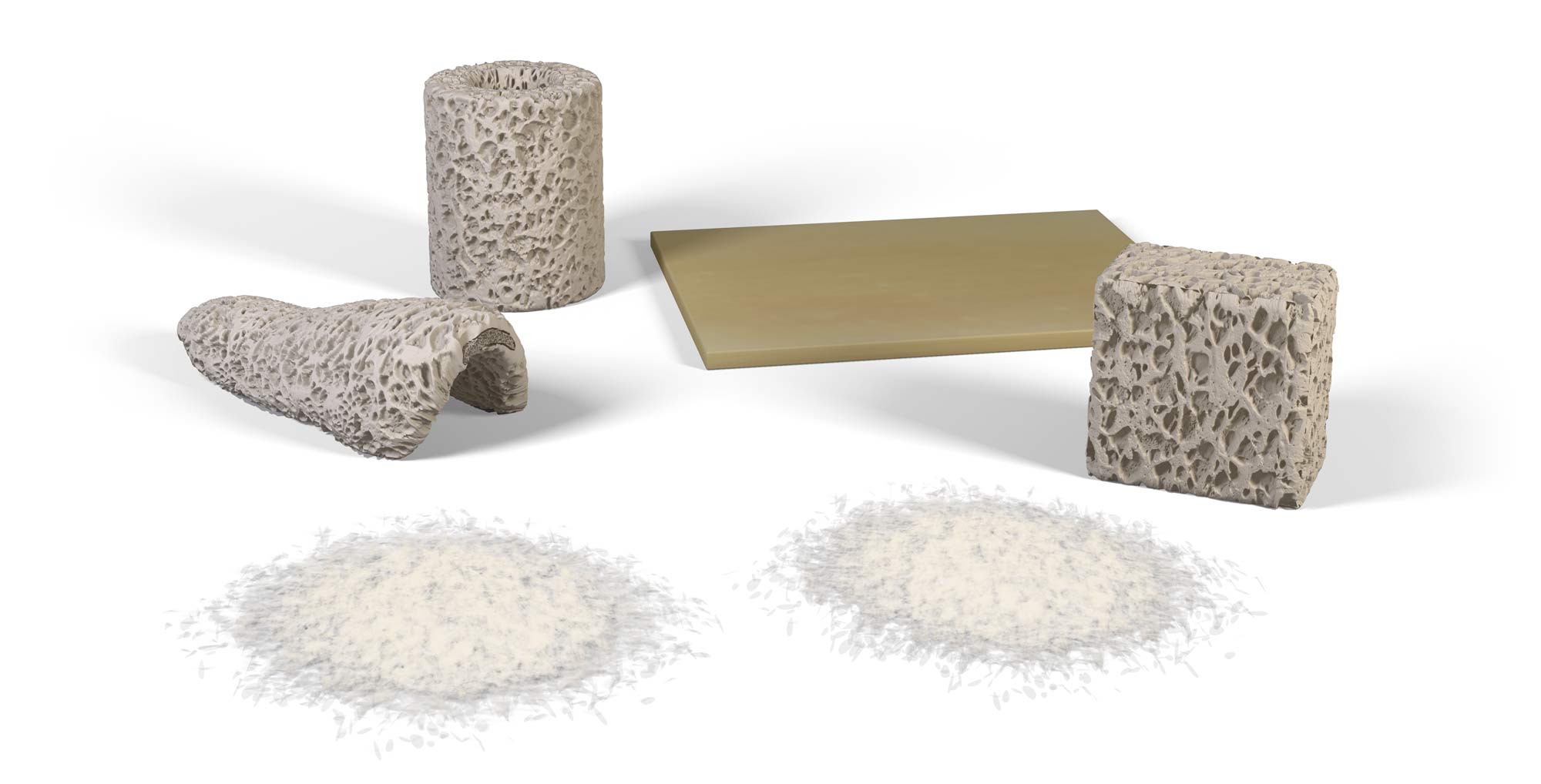
I use Maxgraft for most of my infrabony defects. This includes extraction sockets, for its fairly fast and reliable turnover into natural bone, while maintaining volume stability. Whenever I want to gain volume outside of the bone contours, my biomaterial of choice is Cerabone.
It provides space maintenance and a long-term scaffold for tissue growth, plus it’s very hydrophilic. In addition, the Jason membrane is perfect combined with Maxgraft or Cerabone for guided bone regeneration procedures.
Reducing potential bone loss when using any implant placement technique is important, but it is crucial with regards to immediacy. Also make sure you have access to an array of biomaterials you can trust to support outstanding clinical outcomes.
Reference
Tan WL, Wong TL, Wong MC, Lang NP (2012) A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res 23 Suppl 5: 1-21
This article first appeared in Irish Dentistry magazine. You can read the latest issue here.